Drug Treatment Crisis Grows in West Virginia, But State Just Looks Toward More Punishment
Amid record overdoses, lawmakers ignore calls to restore pandemic-era Medicaid policies expanding access to treatment. They used this session to debate ratcheting up penalties.
Alex Burness | March 7, 2024


In the months leading up to her death, Ashley Omps of Charleston, West Virginia, felt ashamed to be taking suboxone. It was prescribed to her to treat opioid dependency by limiting cravings and withdrawal symptoms, and though it was clearly a much healthier alternative to the pills and heroin she’d been taking before, she hated that she had become reliant on it. Omps felt like she’d replaced one dependency with another.
“I’ve never been sober a day or two since I was 16,” Omps, who was 34, texted her sister on Oct. 5 of last year. “I do not want to be addicted. I fucking hate needing something to feel normal. I might as well actually get high if I’m going to be an addict.”
Though she resented the suboxone, people close to her said it was crucial to her recovery from substance use disorder. And so it was catastrophic that she could no longer obtain it, midway through 2023, after she was kicked off Medicaid.
At the onset of COVID-19, the federal government suspended normal rules for Medicaid to keep people from losing coverage during the pandemic, allowing recipients, including Omps, to go three years without having to demonstrate eligibility. But that policy ended in March 2023, and Omps and millions of others across the country were swiftly dropped from government coverage—for instance because they forgot to file for renewal or made a mistake on their paperwork, or because they had moved to a new state or started earning too much money to qualify for Medicaid. In West Virginia, this change was compounded by the existing staffing and funding challenges in the state’s Medicaid office, and the legislature’s inaction to avert this cliff.
In 2022, Omps started working at the nonprofit West Virginia Family of Convicted People, where she organized events to protest and raise awareness about conditions inside West Virginia’s deadly jails. The job paid $22 an hour, which put her in a difficult spot: She was making too much money to stay on Medicaid, but the job didn’t provide health insurance and Omps couldn’t afford to pay out-of-pocket for her drug treatment.
“She had to go off of suboxone and that is what put her body under a lot of stress,” Omps’ sister, Victoria Omps, told Bolts recently. “It was so hard on her, because of how expensive it was going to be to stay on.”
Already in withdrawal from hard drugs, Omps suddenly found herself in withdrawal from the medication that was treating her addiction. On Oct. 18, she entered the steam room of a YMCA in Charleston, West Virginia’s capital city, then collapsed and died as she got up to leave. She was 34 years old, and though she officially died of a heart attack, Victoria and others who knew Ashley told Bolts they have no doubt about what killed her.
“I think it was entirely about her having to come off of suboxone,” Victoria said. “The withdrawal was so hard. That was the reason she was even in the steam room, so she could try to sweat it out of her pores.”
The so-called unwinding of Medicaid coverage has, as of late last month, led to the disenrollment of more than 17 million Americans, according to a Kaiser Family Foundation analysis. West Virginia has been hit particularly hard: It is one of the poorest states in the country, and thus has one of the highest rates of Medicaid enrollment. The return to normal Medicaid rules has led to the removal of nearly a quarter of all West Virginians who’d been enrolled as of last spring, the Kaiser analysis shows.
Those who work in drug treatment and addiction recovery in West Virginia say this drop-off in coverage has endangered people with substance use disorder and compounded a larger crisis in a state that has already led the country in overdose death rate every recorded year since at least 2014, according to federal data.
As patients like Omps lost access to addiction treatment, advocates pressed state leaders to expand Medicaid eligibility and treatment options in the state. Instead, even in the face of this crisis for drug treatment and recovery, many West Virginia lawmakers have turned to a different approach, pursuing new punishments for people addicted to illegal drugs in a state that already incarcerates more people for drug possession than for almost any other charge.
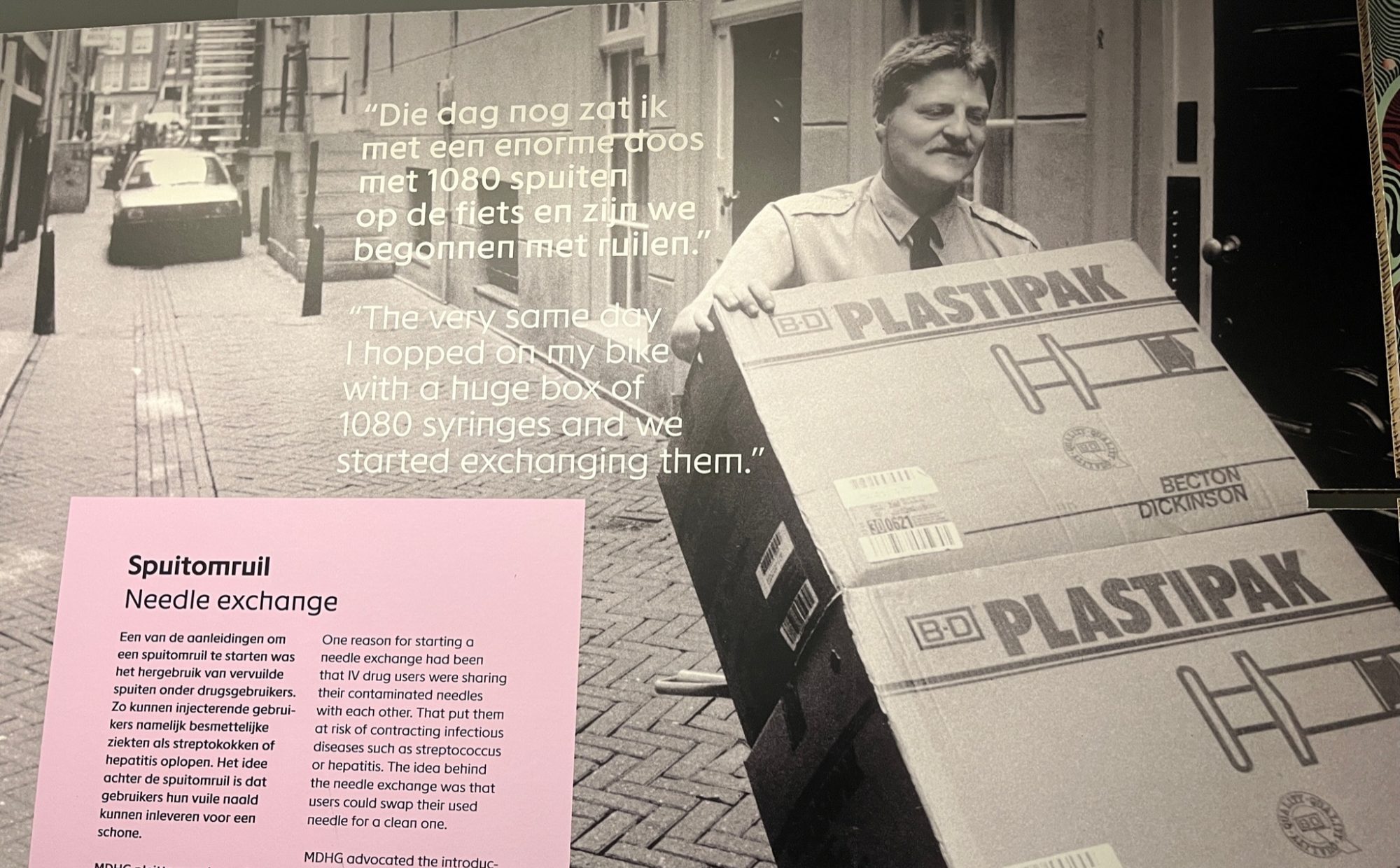
The state legislature, which is controlled by Republican supermajorities, already restricted syringe exchange programs in 2021; this year, it considered bills to outlaw syringe exchanges entirely, as well as to ban methadone—a medication that treats opioid addiction, as suboxone does—and the distribution of clean drug supplies. West Virginia lawmakers also have repeatedly advanced legislation to turn simple drug possession from a misdemeanor to a felony offense punishable by up to five years in prison.
“We’re trying to be proactive here,” Republican state Senator Vince Deeds, the sponsor of that proposal, told Mountain State Spotlight in January. “Right now, if you have someone go in for simple possession, they’re back out and they’re committing more crimes to feed their habits. The idea here is to have early intervention with these end-level users.” (Deeds did not respond to multiple requests for comment from Bolts.)
Deeds’ bill passed the state Senate both in 2023 and this January, but it stalled in a House committee last week as lawmakers declined to pass it. Instead, House Republicans decided to study higher penalties for drug possession in the future, which would push this focus on increased penalties into coming years.
Many who advocate for those struggling with addiction in West Virginia feel frustrated seeing lawmakers focus during their limited time—the 2024 session is already set to end this week—on such solutions. These advocates argue that treatment offers more public safety benefits than harsher punishment, a position bolstered by years of research showing that incarceration does not deter drug use.
“Instead of putting the money and funds into increasing access to treatment, increasing resources and funding to organizations helping with drug treatment, they’re talking about throwing good money after bad by increasing penalties and increasing incarceration rates,” said Kenneth Matthews, a recovery coach who is himself in long-term recovery from addiction.
“There’s not enough money put into treatment facilities,” he said. “Never in the history of people committing crimes has anybody in the midst of their substance use said, ‘Oh, they just increased the penalty, so I’m not going to do this.’ As someone who was formerly incarcerated and in long-term recovery, when I was in the midst of substance use I wasn’t following the legislature and I really didn’t care.”
David Foley, the chief public defender in Mingo County, a rural area in the southern part of West Virginia that The Guardian once called “the opioid capital of America,” said he sees a host of other criminal charges that seem to stem from untreated addiction. “I see so many crimes where, if they are not drug offenses, they are fueled by the desire to get money to get drugs, or it’s people so down on their luck because of drugs,” Foley said. “It just seems like the entire spectrum of criminal charges are in some way influenced by substance abuse.”
Mingo County Sheriff Joe Smith, a Republican, confessed that he sometimes wonders whether arrests and incarceration for certain drug charges are doing any good for people suffering addiction. Smith told Bolts that he and his deputies often arrest the same people over and over again for the same drug-related crimes, and added that even if he could arrest every single person who sells drugs in the area, he doesn’t think Mingo County could solve its problems related to addiction through enforcement alone.
“Out of every crime we work, 80 percent is drug-related. We’ll arrest someone who stole grandma’s earrings, but when you get to the root of it, it was to sell the earrings for a hit of meth or some fentanyl,” Smith said. “It’s a sad situation. I’ve arrested people, and arrested their kids, and worked overdoses off people who I’ve begged to get help.”
Overdose deaths are a regular occurance in Mingo County, which has a population of just over 20,000. Rebecca Hooker, who runs a social services organization in the county, told Bolts that, recently, on a single day in a single 10-mile radius, her community saw four people die of suspected overdoses. “The people in the sector of harm reduction or prevention or rehabilitation really need more money,” Hooker said. “Right now it’s just catch and release.”
Matthews said his work as a recovery coach is particularly difficult these days, now that he must contend with the fact that many of his clients, who are already at high risk of incarceration or overdose—or both—are also trying to navigate the ongoing Medicaid mess. He talked about one client who had to leave a treatment facility because they lost Medicaid coverage, then spent months re-establishing eligibility, only to find that the treatment facility had no bed space for him to return.
“I was worried he’d have a fatal overdose,” Matthews said. “People lost their health care and had to leave their residential programs because they no longer had the ability to pay for it through Medicaid. Some of them were able to hold on and some were not.”
West Virginia’s state Medicaid office has faced criticism for not doing enough to help people keep coverage after the rules changed. In a letter last summer, the federal Centers for Medicare and Medicaid Services admonished the state for keeping people on hold for long periods of time when they called in for help, and warned that this and other forms of administrative dysfunction would lead to many eligible people losing coverage.
Rhonda Rogombe, health and safety net analyst for the West Virginia Center on Budget and Policy, said administrative hurdles have been a particular problem for people needing treatment for substance use disorder. “This is a very vulnerable group of people,” she told Bolts, “and they’re being disconnected from programs they were enrolled in, or could be eligible for.”
Deborah Ujevich, who works at a detox facility outside Charleston, and was close with Ashley Omps, says people have been scrambling over the past year to find addiction treatment after losing Medicaid coverage. “People would call us for a bed and you look their Medicaid up with the system, you go look at member eligibility, and you see no enrollment found,” Ujevich said. “So you can’t take them, and they can’t get meds because the pharmacy isn’t going to fill their protocol.”
Omps’ death while searching for treatment was sadly not unique, Ujevich said, adding, “We have had a number of past patients die because they aren’t getting the care that they need.”
She finds it frustrating that the state continues to pursue harsh enforcement despite little evidence that incarceration is helping to stem substance abuse, especially after so many lost access to addiction treatment under Medicaid.
“They are doubling down here on bad policy and they are not taking into consideration what is actually happening. It’s very, very, very out of touch,” Ujevich said. “We’re really going backward.”
Sign up and stay up-to-date
Support us
Bolts is a non-profit newsroom that relies on donations, and it takes resources to produce this work. If you appreciate our value, become a monthly donor or make a contribution.